First Parish to host weeklong forum on end of life issues

Jane Eckert read an article on this question by Scott Helman in the April 2012 Boston Globe Magazine, and she was so moved by the story that she decided to bring an idea to her minister at First Parish in Lexington, Reverend Peter Boullata. “This is something that we never talk about,” Jane says, “that we don’t know how to talk about, and I thought, ‘wouldn’t is be great if we could do something on end of life issues at the parish?’”
They in turn presented the concept to the parish board. The result: an upcoming program called Choices at the End of Life: The Death with Dignity Initiative: A week-long exploration of personal, ethical and practical issues.
“I think that as a religious community,” says Reverend Boullata, “we are uniquely poised to have this conversation. Human mortality—that’s what religion does well.” And, he says, since First Parish is historically the “town church” it felt right to host this conversation with the town.
The forum is open. All are welcome according to Bill McKenney, Chairman of the parish board. “This is a natural fit for our mission.” he explains. “As Unitarian Universalists, we address complex issues with an open mind to seek information and learning. Our congregation really doesn’t have a position on this—if you talked to ten people here you’d probably come up with eight different opinions.” McKenney stresses the importance of “providing a safe and open environment” where he hopes people can disagree and disagree in a way that is respectful. “We want this to be a forum that is informative and supportive for discussing something as difficult as end of life.”
Reverend Boullata agrees, “It’s part of our calling as a faith community to be a venue for people asking questions which are spiritual issues as well as moral issues.”
Jane Eckert is particularly thrilled that they have been able to put together such a well-rounded week of informative sessions with an impressive list of speakers. “We’re hoping to have a diversity of perspectives represented—to see both the differences and the similarities. “Having lived through the past few years where there has been such rancor,” Eckert reflects, “We really want to nurture respect for differences and viewpoints here.”

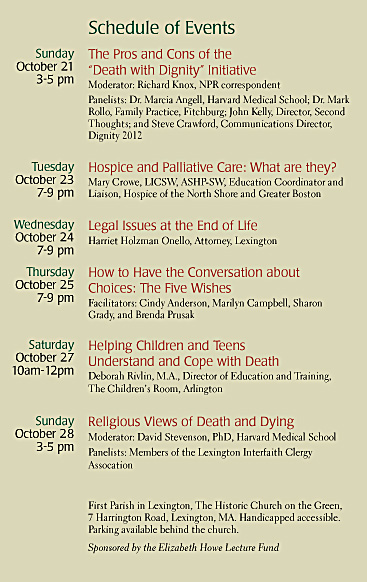
The week will kick-off on Sunday October 21st with a panel discussion on the ballot question moderated by NPR health reporter Dick Knox. Dr. Marcia Angell who has been actively advocating for the ballot initiative will serve on the panel. Dr. Angell, who is a physician and served as the editor of the New England Journal of Medicine, is currently a senior lecturer in social medicine at Harvard Medical School. Dr. Angell was the first of the original 14 petitioners to put the Massachusetts Death with Dignity Act on the ballot in November and is a member of the Massachusetts Death with Dignity Coalition (www.dignity2012.org). Also serving on the panel is John Kelly, a disability rights advocate and Director of Second Thoughts an organized opposition group (www.secondthoughts.org). John has been making the rounds of radio talk shows and forums (he spoke at Jay Kaufman’s last Open House) to add his special perspective to the opposition. Another opponent of the initiative, Mark Rollo, a physician in Fitchburg, Massachusetts will also serve on the panel.
The remainder of the week’s programming will focus on hospice and palliative care, legal issues around end-of-life, the Five Wishes program, talking with children and teens about death and finally the different religious views around death and dying. “We have been very fortunate with our panels,” Eckert says. We wanted to have a mix of professionals and real folk involved—not just people with a professional stake.”
BALLOT QUESTION 2 On Sunday October 21st the initial panel discussion at First Parish will take on the many issues surrounding the Massachusetts Ballot Question 2, Prescribing Medicine to End Life, or the Death with Dignity Act. The law would allow willing doctors to provide a patient with a prescription for drugs that when self-administered will end their life. Many patients have a DNR (do not resuscitate) directive or MOLST (Medical Orders for Life-Sustaining Treatment) orders in place. Both of these documents can direct hospitals, EMS personnel and other healthcare to withhold CPR, or intubation in cases of a life threatening event. Question 2 goes beyond both these instruments by allowing terminal patients to end their own life willfully and lawfully with a lethal dose of medication when and where they choose.
To qualify to receive the life-ending prescription, the patient must have a medical prognosis of six months or less to live. They must be informed by the doctor of all treatment alternatives. The patient must be determined to be competent, the doctor must be willing to participate (doctors can refuse to participate) and the patient must make the request three times including once in writing witnessed by two people (one who is not a relative by blood or adoption). The patient must be capable of ingesting the medicine without assistance. The patient must be an adult and can change their mind at any time. There is a waiting period imposed between requesting the prescription in writing and receiving the script from the doctor. A similar law passed in Oregon in 1997 and Washington State in 2009. The language of the Massachusetts act is virtually identical to the Oregon law. Massachusetts would be the first state on the East coast to approve the measure if it passes which means all eyes are on Massachusetts as a test case for advancing the law to other states.

The Massachusetts Medical Association (MMA) is opposed to Question 2. They argue that the proposed safeguards against abuse of the law are inadequate. On their website (www.massmed.org) the MMA outlines their opposing position saying, “Enforcement provisions, investigation authority, oversight, or data verification are not included in the act.” The MMA position paper ends with a quote from past president Dr. Lynda Young who states that “physician assisted suicide is incompatible with the physician’s role as a healer.”
Proponents of the measure like Dr. Marcia Angell disagree with the MMA position. In response to an email inquiry Dr. Angell wrote, “I think nearly everyone knows someone who has died a lingering, difficult death, despite state-of-the-art palliative care. Some of these patients would like the choice of ending their lives sooner and more peacefully. The Death with Dignity Act, which will be Question #2 on the November ballot, would give Massachusetts the same law that has worked well in Oregon for the past 14 years, and is now supported overwhelmingly by the public in that state.”
Dr Angell stresses the matter of personal choice, “It would permit dying patients in Massachusetts, with no more than six months to live, to ask their doctor for a prescription for medication that would allow them to die more peacefully, if — and only if — they choose, and if their doctor agrees. This would be an option, not a requirement, for both dying patients and their doctors. Most patients with terminal illness, of course, will not need this law, but some will, and I see no reason to require suffering patients to continue an agonizing, inexorably downhill course against their wishes.”
John Kelly sees the downhill course differently. I spoke by phone with John who is a passionate opponent of the measure. As a disabled person (a quadriplegic due to an accident early in life) and a disability advocate, John worries that independence, autonomy are equated with worthwhile quality of life in this argument. “We see this as a direct threat when the characteristics of our own lives are justification for state-supported suicide.”
Since disabled people are to varying degrees dependant on other people for their care, Kelly also believes that this characterization would send a dangerous message to the disabled. “This bill does not solve that problem. The real problem is that some people don’t get the care that they deserve or the social support that is necessary,” he says.
Critics of the bill worry about everything from incorrect diagnoses, callous profit-driven insurance companies, and cash-strapped families exerting pressure on sick family members because they can’t afford care or greedy heirs that may want to hasten their inheritance.
As part of their law, the Oregon Heath Authority has been required to do surveillance and to issue yearly reports. So far, Oregon’s data has not shown cause for alarm. The median age for those ingesting the medication was 71 in 2011. Most were white well-educated cancer patients; some had A.L.S. Only 1 person of the 71 was referred for a psychiatric evaluation. Doctors’ reports from Oregon indicate that people were most concerned with their quality of life, specifically the inability to participate in enjoyable life experiences (90.1 %), loss of autonomy (88.7%) and loss of dignity (74.6). Fear of pain does not seem to be a driving concern for those seeking the life-ending prescription. The data shows that remarkably few people actually take advantage of the law. In 2011, 114 individuals requested a life-ending prescription and 71 of those individuals actually died from the self-administered dose. However, use of the option has increased since its inception. In 1998 only 16 people died from the prescription they had requested. [Source:http://public.health.oregon.gov/ProviderPartnerResources/EvaluationResearch/DeathwithDignityAct/Documents/year14.pdf]
PALLIATIVE CARE & HOSPICE CARE For many in the medical community, the answer is palliative care and hospice not physician-assisted suicide. Palliative care and hospice provide for comfort and give the patient the ability to die at home. Most agree that there has been a tremendous amount of progress around the practice of palliative care which provides pain management, anxiety relief, psychological support and panoply of alternative treatments. All of these alternatives are designed to help the dying patient make the most of their last days with the least amount of suffering. This will be the topic of the Tuesday forum: Hospice and Palliative Care-What are they? The program runs from 7-9PM.
Advocates of the Death with Dignity Act feel that palliative care and hospice can exist in harmony with the proposed law. Dr. Angell, who has been articulating the proponent argument around the state over the past few months often, turns the opposition argument on its head. When asked by local NPR host Callie Crossley why she supported the initiative, Dr. Angell said, “Why would anyone—the state, organized medicine—anyone be against it? You should let the patient decide when palliative care and hospice are over.”
Some experts feel that adopting the DWDA in Oregon has created better palliative care in the state because doctors want to make sure that a life ending prescription is truly a last resort for the patient.
A COMPLEX QUESTION A recent Suffolk University poll (http://www.suffolk.edu) of likely Massachusetts voters indicates that 64% of Bay Staters are in favor of the Prescribing Medication to End Life law, or Question 2. Western New England University Polling Institute conducted a poll in May showing 60% in favor.
Anyone who has been following this issue knows that it is a big topic with many overlapping themes, emotional hot buttons, religious implications and medical and legal repercussions. What makes good social policy? Good law? If it doesn’t affect your personal choice, should it matter if others have the ability to choose differently? And what about mistakes? What is the proper role of religion in this discussion? Can well meaning laws have unintended social consequences? Is it ever morally acceptable to hasten death?
These are some of the questions that will be explored at the Sunday forum and it is your chance to ask questions and think deeply about this difficult issue right here in Lexington among friends and neighbors.
“One of the things we Unitarians do well is that we talk. We don’t always agree, but we talk,” says Jane Eckert. “Even if you don’t come to the first night, there’s so much going on during the week including a night on how to talk about death with children.” Bill McKenney says, “Our hope is that people will come out and join us so we can all learn together.”
“We need to puncture those bubbles—that taboo.” adds Reverend Boullata, “I am hoping that people will begin to have some sense of what it means to die well, to begin thinking ‘How do I want to spend the last weeks and days and hours of my life and what will it mean to be well cared for in that circumstance?’ Maybe in a small way this week of programming will help with that.”
